Plantar Fasciitis
Plantar fasciitis
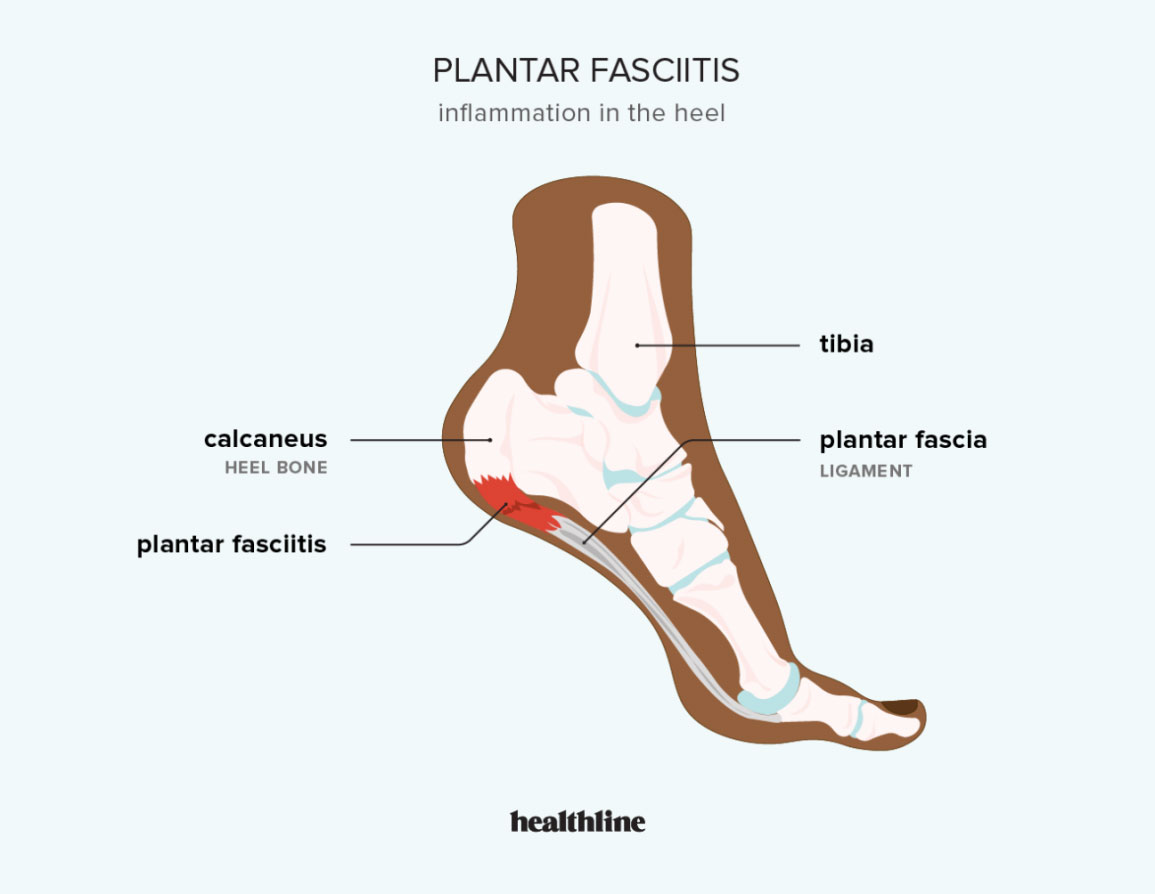
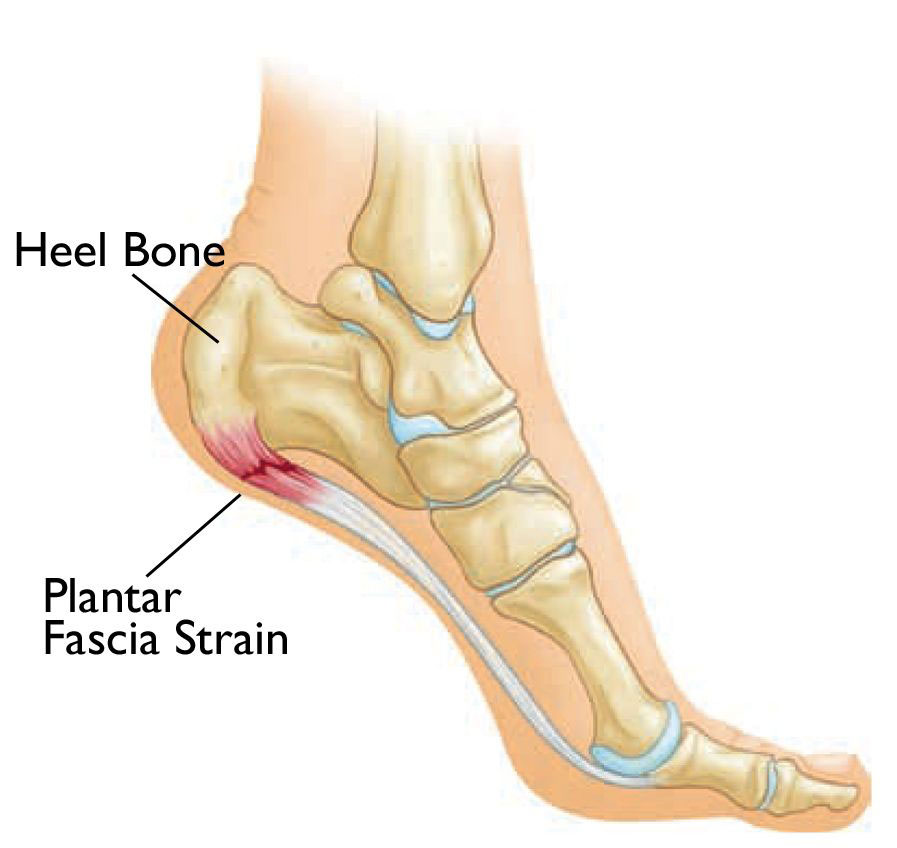
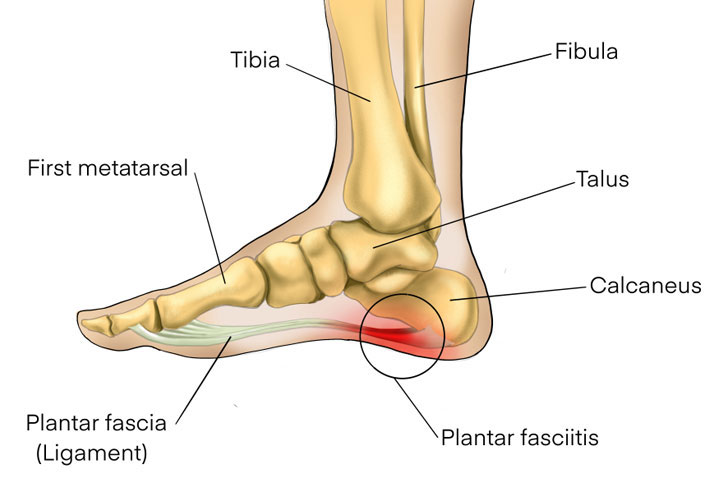
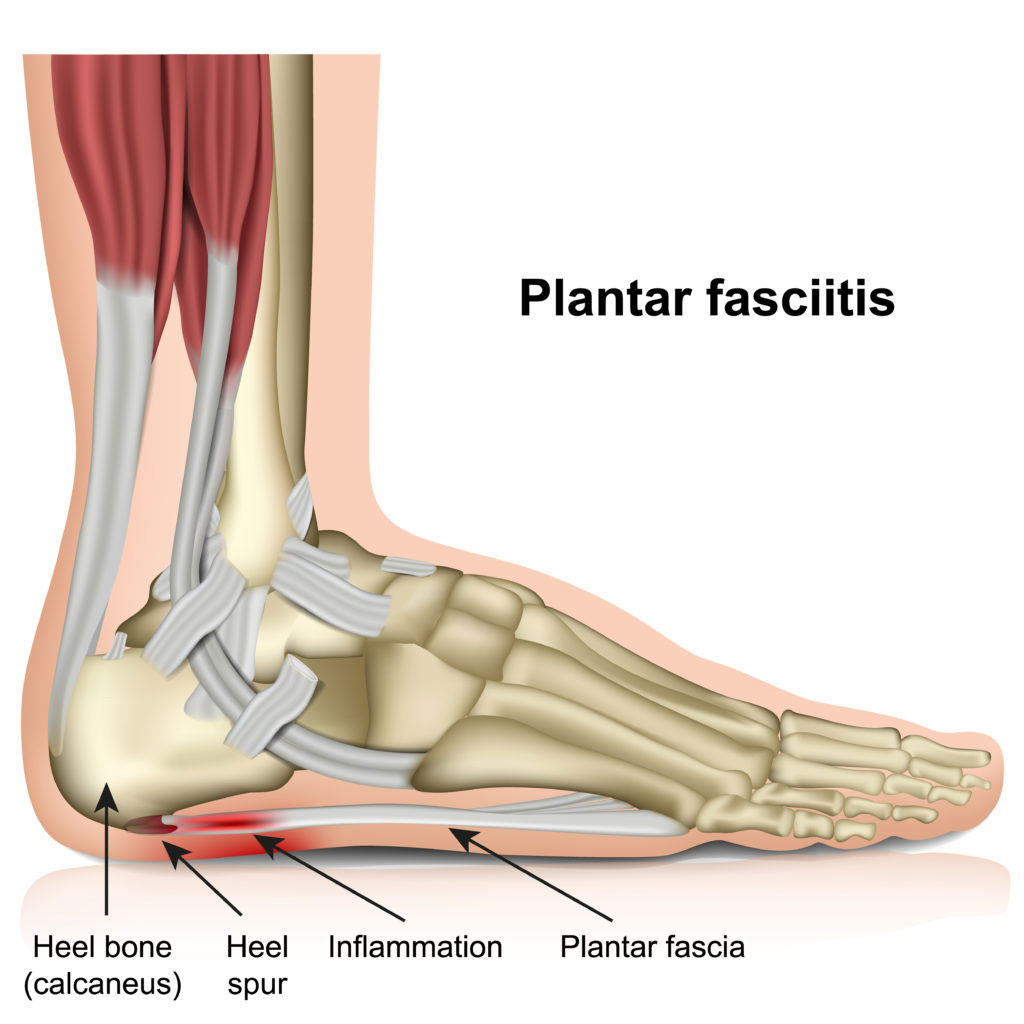
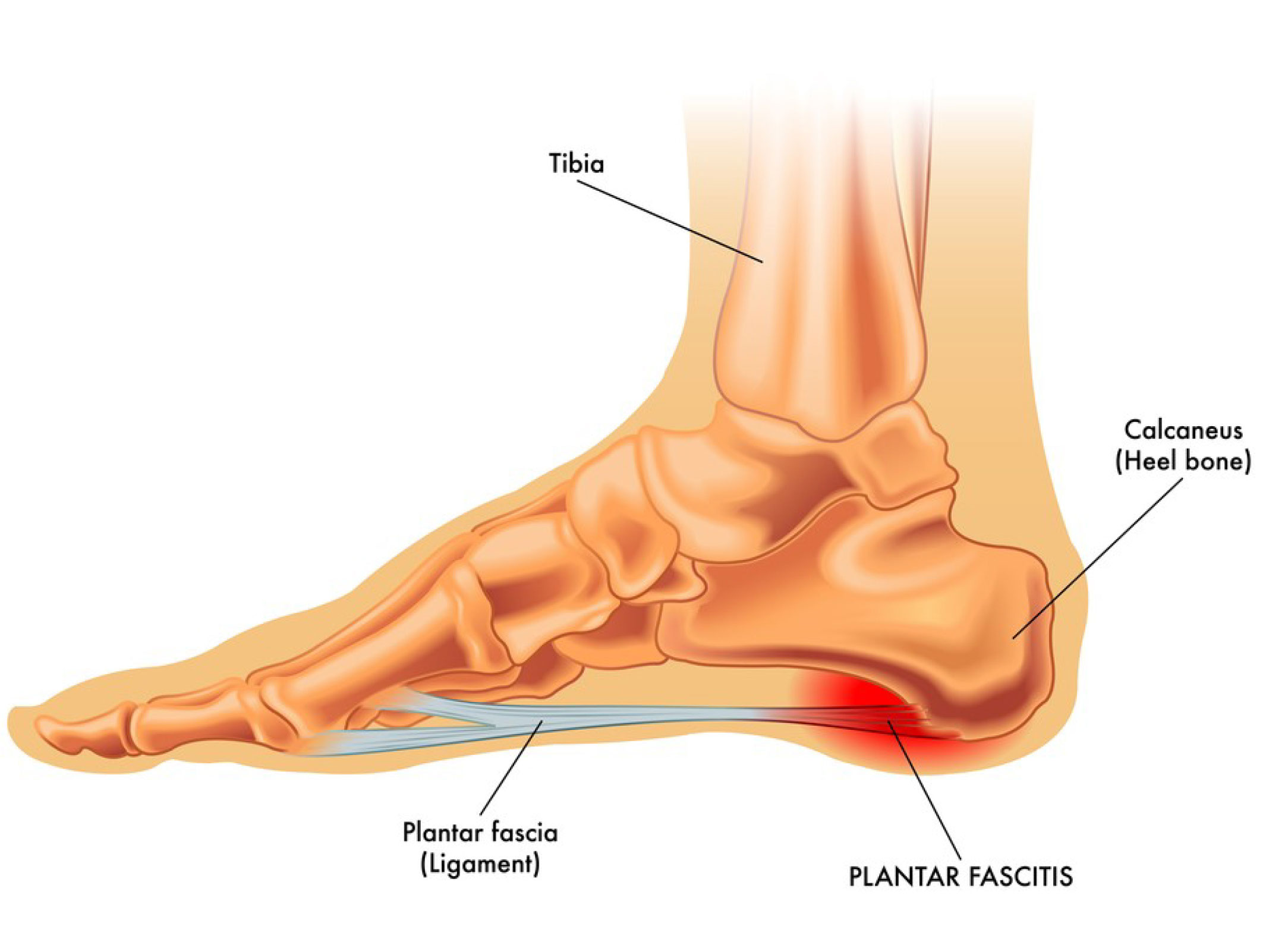
Do you ever experience heel pain? If so, it could be due to plantar fasciitis. Plantar fasciitis is inflammation of the connective tissue that runs from the heel to the toes. This can cause a great deal of discomfort, making it difficult to walk or stand for any length of time. Fortunately, there are several treatment options available that can help reduce inflammation and ease the symptoms. Keep reading for more information on plantar fasciitis and how to treat it.
What are the symptoms of plantar fasciitis?
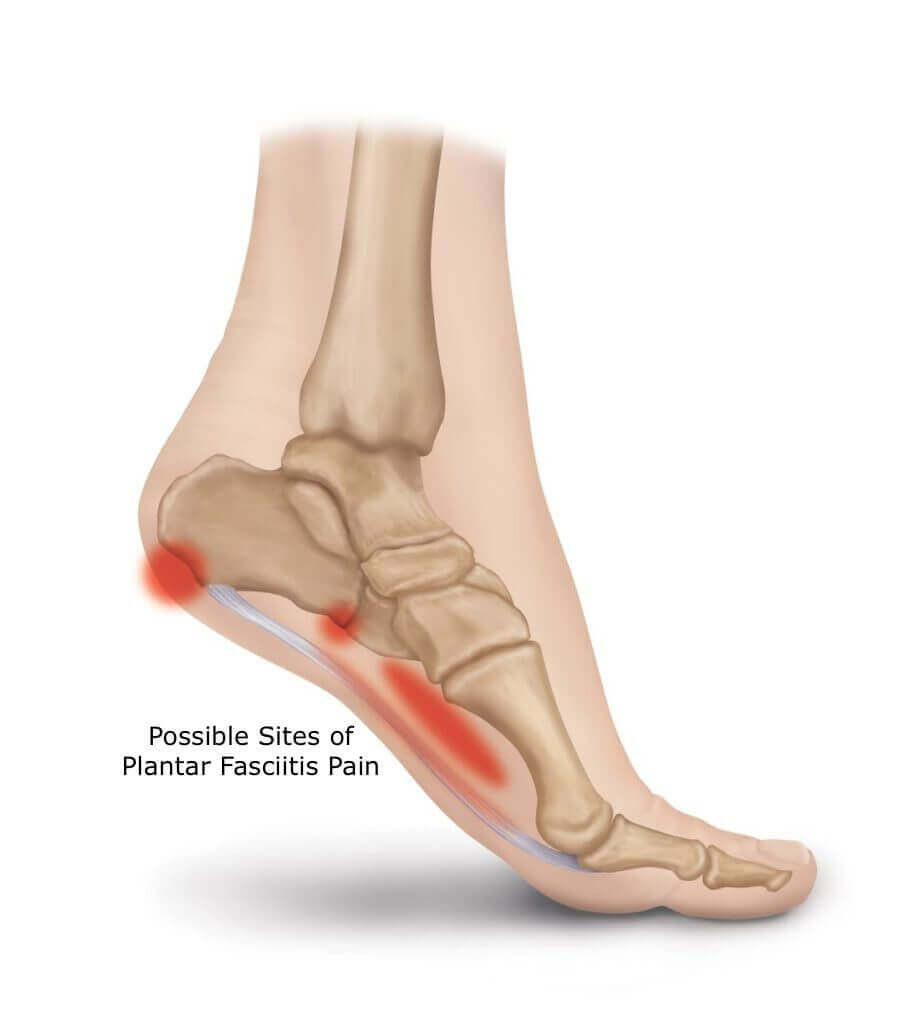
The symptoms of plantar fasciitis include heel pain and stiffness, pain in the arch of the foot, and pain with walking or standing. The pain is often worse in the morning when you first get out of bed. Plantar fasciitis is caused by inflammation of the plantar fascia, the band of tissue that extends from the heel to the toes.
What causes plantar fasciitis and how can you prevent it?
Plantar fasciitis is a condition that leads to pain in the heel and bottom of the foot. It is caused by inflammation of the plantar fascia, the connective tissue that runs along the bottom of the foot. Plantar fasciitis is common among runners and other athletes who put repetitive stress on their feet. It can also be caused by obesity, poor footwear, or an uneven walking surface.
There are several things you can do to prevent plantar fasciitis, including:
-Wearing shoes that provide good support for your feet
-Stretching your calves and Achilles tendon regularly
-Use orthotics or arch supports if you have flat feet or high arches
-Maintaining a healthy weight

Diagnosis for plantar fasciitis
The diagnosis for plantar fasciitis is typically based on a person’s medical history, physical examination, and description of symptoms. Imaging tests may be used to rule out other causes of heel pain, such as a stress fracture or bone spur. Plantar fasciitis is usually diagnosed using a combination of a person’s medical history, physical examination, and description of symptoms. Imaging tests, such as X-rays or magnetic resonance imaging (MRI), may be ordered to rule out other causes of heel pain, such as a stress fracture or bone spur. A doctor may ask the following questions:
- When did you first begin experiencing heel pain?
- Do you have pain upon rising in the morning?
- Does the pain improve with activity or worsen with activity?
- Do you have pain that is worse with certain types of shoes?
- What, if any, home remedies or self-care measures have you tried to relieve your heel pain?
- Have you had plantar heel pain before? If so, how was it treated?
- Do you have any other medical conditions apart from chronic heel pain?
- Do you take any medications regularly?
In addition to a complete medical history and physical examination, diagnostic tests for chronic plantar fasciitis may include the following
X-ray
A diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
MRI
A diagnostic procedure that uses a combination of large magnets, radio frequencies, and a computer to produce detailed images of organs and structures within the body.
Bone scan
A diagnostic procedure that uses a radioactive substance to examine the condition of bones.
Ultrasound.
A diagnostic technique that uses high-frequency sound waves and a computer to create images of blood vessels, tissues, and organs.

Treatment of Plantar Fasciitis
Normal Cases
If you do develop plantar fasciitis, there are treatments that can help relieve the foot pain, including:
-Resting your feet
-Applying ice to the affected area
-Stretching and doing exercises specifically designed for plantar fasciitis
-Taking over-the-counter anti-inflammatory medications such as ibuprofen or naproxen
Severe Cases
To treat plantar fasciitis of severe nature, more aggressive treatment may be necessary, such as:
-Physical therapy
-Corticosteroid injections
-Extracorporeal shock wave therapy (ESWT) – a non-invasive treatment that uses sound waves to stimulate healing
-Surgery, though this is rare and typically only considered as a last resort
If you are experiencing pain in your heel or bottom of your foot, be sure to see your doctor get a proper diagnosis. With the right treatment, you can get relief from the pain and get back to your normal activities.
Recovery from Plantar Fasciitis
Plantar fasciitis affects your foot negatively thereby causing heel pain and other problems with the foot. The plantar fascia ligament is a band of tissue in the foot that connects the heel bone to the toes. This condition occurs when the plantar fascia becomes damaged or inflamed.
Plantar fasciitis is a common condition, and it can be difficult to treat. However, there are some things that you can do to help ease the pain and speed up the healing process.
Rest:
One of the best things that you can do for plantar fasciitis is to rest your feet. This means taking a break from activities that put strain on your feet, such as running or standing for long periods of time. You may need to use crutches or a walking boot to keep weight off of your feet while they heal.
Ice:
Applying ice to the affected area can help reduce inflammation and pain. Ice should be applied for 15-20 minutes at a time, several times a day.
Stretching:
Stretching the muscles and tendons around the foot can help ease pain and promote healing. There are a number of stretches that can be beneficial for plantar fasciitis.
Arch supports:
Wearing arch supports and shoe inserts can help take pressure off of the plantar fascia and ease the pain. Arch supports can be bought over-the-counter or custom-made by a podiatrist
How to stretch your feet and calf muscles for relief from Plantar Fasciitis
1. Heel stretches.
Sit on the floor with your legs extended straight in front of you. Place a towel around the ball of your foot and pull gently back toward your body to stretch the bottom of your foot. Do this several times.
2. Toe stretches.
Sit on the floor with your legs extended straight in front of you and place a band around your big toe. Gently pull the toe toward your body to stretch the top of your foot and hold for several seconds. Repeat with each toe.
3. Calf stretches.
Stand with your hands against a wall and one leg behind the other, far enough back that you can feel a stretch in your calf muscle when you keep your heel on the ground. Keep your back leg straight and your front knee bent as you lean into the wall. Hold for 30 seconds and repeat with the other leg.
4. Achilles tendon stretches.
Stand with one leg in front of the other, keeping your back leg straight and your front knee bent. Lean forward onto your front leg, keeping your heel on the ground, to stretch your Achilles tendon. Hold for 30 seconds and repeat with the other leg.
5. Plantar fascia release
Sit on the floor with both legs extended straight in front of you and a belt or towel around the ball of one foot. Gently pull on the towel to stretch the plantar fascia (the connective tissue that runs along the bottom of your foot). Hold for 30 seconds and repeat with the other foot.
If your stretching and exercises don't provide relief, or if the pain is severe, be sure to see your doctor. Patients with plantar fasciitis may need more aggressive treatment, such as corticosteroid injections or extracorporeal shockwave therapy. In rare cases, surgery may be necessary. But with the right treatment, you can get relief from plantar fasciitis pain and get back to your normal activities.
Plantar Fasciitis in children
Plantar Fasciitis in children can be caused by a number of things, including:
– trauma to the foot, such as from a fall or car accident
– overuse of the foot, such as from playing sports
– obesity
– flat feet
– high arches
– tight calf muscles
– shoes that don’t fit properly or offer enough support
For treating plantar fasciitis in children, measures may include:
– icing the foot several times a day to reduce pain and inflammation
– stretching exercises to loosen the tissue around the heel
– physical therapy
– night splints
– orthotic devices, such as arch supports or heel pads, to help support the foot
– prescription medications to reduce pain and inflammation
– surgery, although this is a rare plantar fasciitis treatment. In most cases, plantar fasciitis in children can be treated successfully with a combination of rest, ice, and stretching exercises. Surgery is rarely needed.
If your child has plantar fasciitis, be sure to have them wear comfortable shoes that offer good support. You may also want to have them use an over-the-counter pain reliever, such as ibuprofen, to help reduce pain and inflammation. If the pain is severe or persists, be sure to talk to your child's doctor.
Are heel spurs different from Plantar Fasciitis?
There is a lot of confusion out there about heel spurs and plantar fasciitis. Heel spurs are often blamed as the source of heel pain, but in reality, they are only a symptom of another underlying issue. Plantar fasciitis, on the other hand, is a condition that can cause heel pain (among other symptoms). So, what’s the difference?
Heel spurs are bony growths that form on the heel bone. They are most often caused by repetitive stress injuries, such as those associated with running or dancing. In some cases, they can also be caused by arthritis or structural defects in the foot. Heel spurs do not always cause pain, but when they do, it is usually due to the inflammation of surrounding tissues.
Plantar fasciitis is a condition that results in pain and inflammation in the plantar fascia, the band of tissue that runs along the bottom of the foot from the heel to the toes.
Plantar fasciitis is often caused by overuse or repetitive stress injuries, but it can also be caused by structural problems with the feet, such as high arches or flat feet. In some cases, plantar fasciitis can also be caused by arthritis.

Have you been injured at some point in your journey?
Are you not achieving your highest level of function?
We’ve helped hundreds of people at all walks in life
get back to performing their best painfree!
3 Ways to Level Up Your Rehab and Injury Prevention With Us